Jens G Brockmann, Saudi Arabia
Director Intestinal Transplantation, Consultant Abdominal Transplantation
Organ Transplant Center of Excellence
King Faisal Specialist Hospital and Research Center
Pancreas after kidney transplantation in Saudi Arabia providing excellent recipient and renal allograft survival
Jens G Brockmann1, Dieter C Broering1, Hassan AlEid1, Ahmed Zidan1, Ehab H Abufarhaneh1, Tariq Ali1.
1Organ Transplant Center of Excellence, King Faisal Specialist Hospital and research Center, Riyadh, Saudi Arabia
Introduction: PAK is criticized compared to continued insulin therapy for increasing risks of renal graft loss and higher mortality early after transplantation
Methods: The pancreas transplant program at KFSH&RC, Saudi Arabia was restarted in December 2014. All recipients of either SPK or PAK, including retransplants received exocrine drainage into the third part of the recipient duodenum.
Prospective data collection approved by the Research Advisory Committee (“Organ Transplant Registry”, RAC 2121012). This study being a retrospective analysis of an approved standard operative procedure did not require additional ethical review.
Results: 23 pancreas after kidney transplants have been perfomed in 20 recipients from 12/2014 until 04/2023. All recipients underwent living donor KTX 3.9 years (median; range 0.5-23) prior PAK. Median time of insulin dependency prior pancreas transplantation was 22.6 years (range,13.5–40.5 years). PAK recipient average age at time of transplant was 35.4 years, sex distribution was 17 male : 5 female. The average pancreas donor risk index amounted to 1.78. Patient survival at a median follow-up of 6.7 years post PAK was 100% .Complete insulin independence at 1,3 and 5 years post PAK was 70, 60 and 55%, respectively. 11 pancreas grafts in 9 recipients were lost due to rejection episodes. One pancreas graft was lost due to early thrombosis at POD 2. In same patient the only renal allograft loss was observed 2.5 years post PAK resulting in an overall kidney allograft survival of 95 percent at follow-up. Three recipients underwent pancreas retransplantaiton with a permanent success rate of 33%. All recipients (n=2) of LD-ABOi kidney transplantation lost their pancreas allograft for immunological reasons at 90 and 1080 days post PAK, respectively.
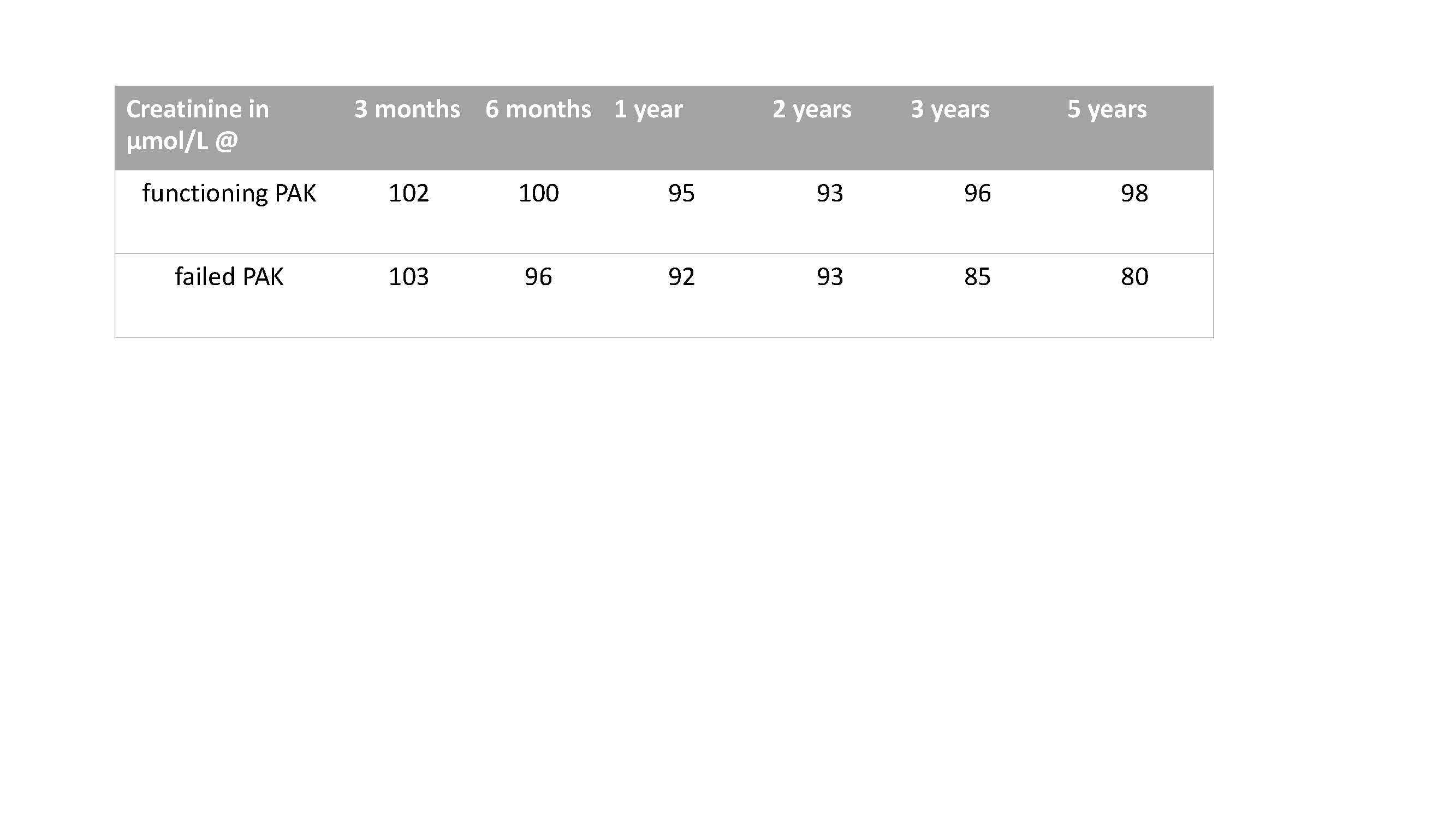
Mean creatinine at time of PAK was 92 µmol/l (range 60-121). There was no statistical difference for creatinine in recipients with fuctioning versus a failed pancreatic allografts at 0.5,1, 3 and 5 years post months PAK or PAK loss, respectively.
PAK pancreas allograft outcome is clearly inferior when compared to simultaneous pancreas and kidney transplantation at the same center (SPK pancreas allograft survival 95% @1 and 3 years and 92% @ 5 years). Given the limited resources of first dialysis and secondly deceased donor organs in a middle eastern country (about 3 deceased organ donors per million population per year) living donor kidney transplantation followed by PAK is a valuable option for patients suffering of end stage renal diesease secondary to diabetic nephropathy. Favourable recipient and renal allograft outcomes are linked to a center based intense follow-up
Conclusion: Despite a very limited organ donor pool providing high risk donor allografts PAK are comparable ti international standars. Mid term renal allograft survial of 97% and a recipient survival of 100% at 6.7 year of follow-up are encouraging.
Lectures by Jens G Brockmann
| When | Session | Talk Title | Room |
|---|---|---|---|
|
Thu-26 18:30 - 20:00 |
Poster Session | Pancreas after kidney transplantation in Saudi Arabia providing excellent recipient and renal allograft survival | Foyer Area |
