Angelika C. Gruessner, United States
Professor of Medicine
Nephrology
SUNY Downstate Medical Research University
Pancreas transplantation – An Option after Total Pancreatectomy without Islet Auto Transplantation (IAT)
Angelika C. Gruessner1, Subodh J Saggi1, Rainer WG Gruessner1.
1SUNY Downstate Health Sciences University, Brooklyn, NY, United States
Introduction: Many patients who lost their pancreas due to a total pancreatectomy are left in a very labile diabetic state. The rate of emergency admissions and the mortality after total pancreatectomy is high due to severe hypoglycemia. For pancreatectomized patients who have not undergone a TPIAT or not even a failed one, a subsequent pancreas transplant is the best treatment option to achieve optimal metabolic control. The group of pancreatectomized patients without simultaneous IAT attempt and subsequent pancreas transplant has not been studied in detail before.
Method: The IPTR/UNOS database was searched for all patients with a diagnosis of total pancreatectomy prior to a pancreas transplant without ever receiving an IAT. A comprehensive description of patients, risk factors, and outcomes is provided.
Results: A total of 57 primary pancreas transplants after total pancreatectomy were performed between 1993 and 2021.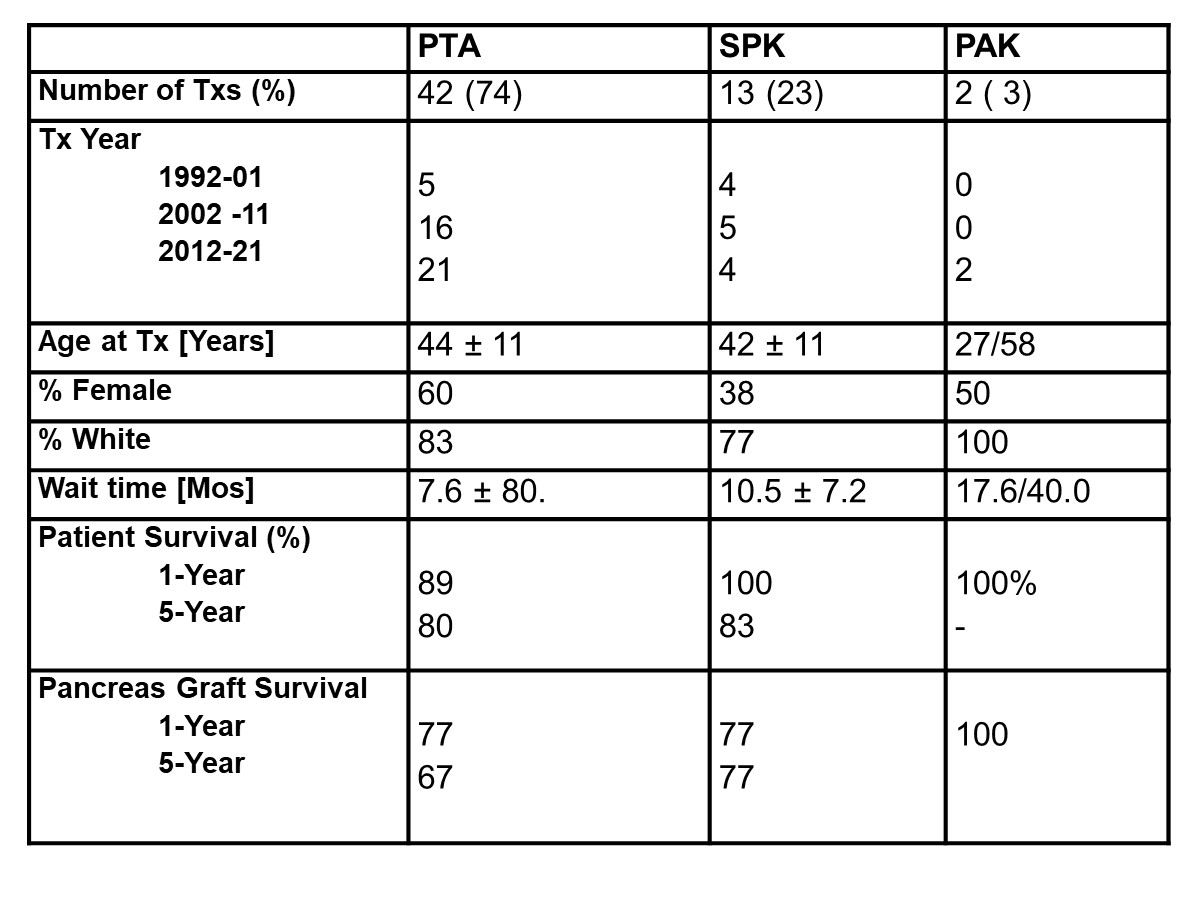
The majority of patients received a pancreas transplant alone (PTA; n=42), followed by a simultaneous pancreas/kidney transplant (SPK; n=13). Only 2 patients received a pancreas after kidney transplant (PAK). Most patients required a total pancreatectomy due to chronic pancreatitis, but 5% had their pancreas removed due to traumatic injuries. Table 1 shows the basic patient and transplant characteristics. The procedures were mostly performed at high volume transplant centers.
The patient survival in all 3 transplant categories was excellent, especially when the very long time span of 30 years is taken into consideration. Pancreas graft survival was also excellent. Of particular interest is the initially high graft thrombosis rate whereas the rate of immunological losses was low.
The most influential factor for PTA graft survival were young recipient age (RR: 20.4, 1.8 – 40.2) and, surprisingly, old donor age (RR: 7.2, 0.80 -59.2). The maintenance protocol with tacrolimus in combination with MMF reduced the risk of graft failure in recent years.
Discussion/Conclusions: This first series of 57 patients who underwent a pancreas transplant after total pancreatectomy without simultaneous IAT shows: (1) higher 1- and 5-year patient survival rates than for pancreatectomized patients without a transplant (Zakaria HM, 2016); (2) similar graft survival rates over 30 years as for non-pancreatectomized patients; and (3) insulin-independence in all patients with graft function. As the results of pancreas transplants in pancreatectomized have significantly improved over time, this treatment option should be offered much more frequently to reduce the 10-20% death rate over time caused by hypoglycemia in non-transplant patients.
