10-year experience of donors after circulatory death for islet transplantation in Scotland
Kenneth Nicoll1,2, A Timpson3, L Irvine3, C Fattah3, D Mitchell3, K Duncan2, S Forbes1,2, J Casey1,2, A Sutherland1,2.
1Transplant Surgery, Royal Infirmary of Edinburgh, Edinburgh, United Kingdom; 2School fo Medicine, University of Edinburgh, Edinburgh, United Kingdom; 3Scottish National Blood Transfusion Service, (NHSBT), Edinburgh, United Kingdom
Introduction: There has been an increase in the proportion of Donors after Circulatory Death (DCD) in both Europe and the USA. However, pancreas utilisation from DCD donors remains low and there is concern that DCD donors may yield poorer islet isolations resulting in fewer transplantations. The Scottish Islet Transplant Unit has performed 325 islet isolations, 61 from donors after circulatory death (DCD) over the last 10 years. This study examines the quality and clinical outcome of islet cell isolations from DCD donors compared to DBD donors.
Method: A database was prospectively maintained of all islet cell isolations from pancreata accepted for clinical islet transplantation from 2012 to 2022. This included demographic and clinical features of donors in addition to quantification of islet yield. Regression was applied to the data based on the binary outcome of meeting the minimum islet yield of 200,000. DCD and DBD populations were also directly compared to assess for demographic differences and outcomes.
Results: On multivariate logistic regression, the following donor variables were considered: DBD or DCD donation, BMI, CMV status, blood group, age, weight, height, BMI, donor amylase, if the organ had previously been considered for whole-pancreatic transplant. None of these factors had a significant impact on meeting clinical release criteria. This result was unaltered when DBD donors were considered in isolation. Nonetheless, BMI, girth, HbA1c and islet purity all correlated significantly with absolute islet yield (p<0.02).
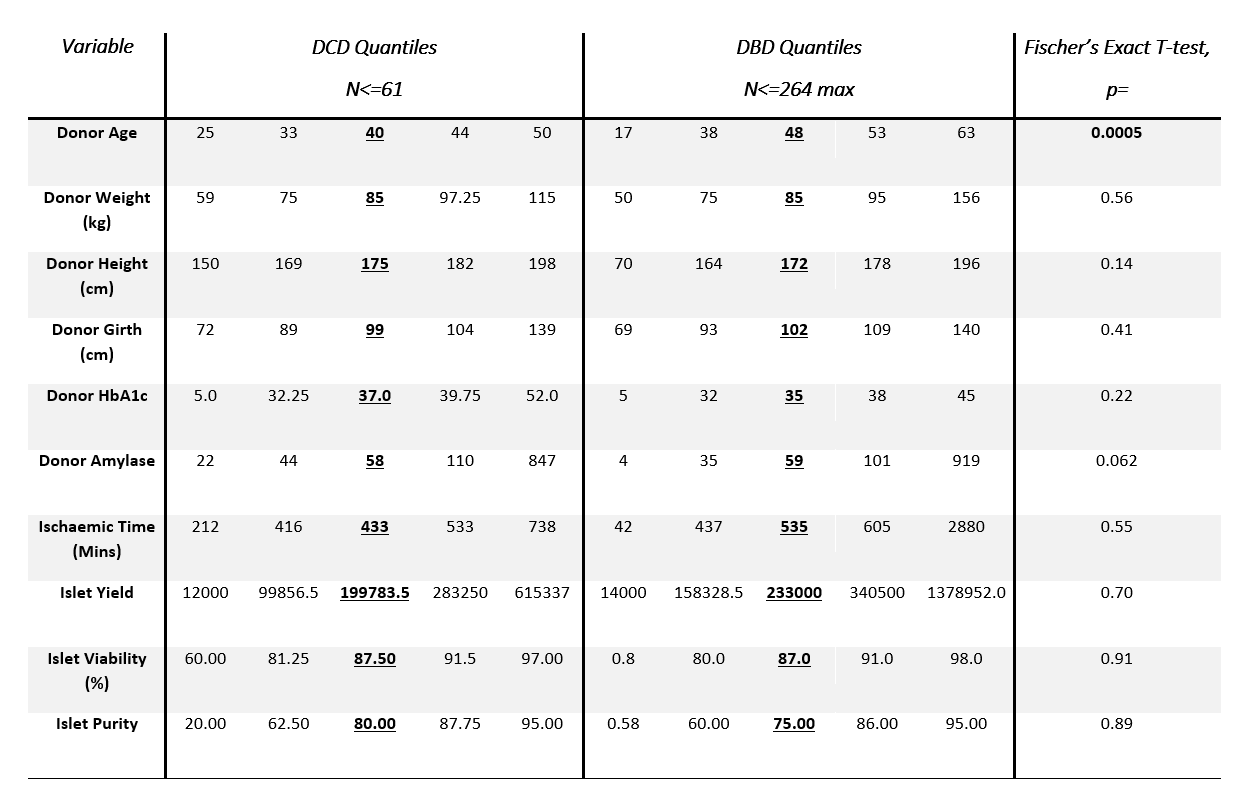
The DBD and DCD populations were well matched except for age, with DCD donors significantly younger (median 40 vs 48, p= 0.0005). Direct comparison of islet yield (median 199784 vs 23300, p=0.7), viability (median 87.5% vs 87.0%, p=0.91) and purity (median 80.0% vs 75.0%, p= 0.89) were not significantly different between DCD and DBD groups. Furthermore, there were no differences in the proportion of isolations from DCD donations that were transplanted (23 from 61, 37.7%) compared to DBD donations (114 from 264, 43.2%), Χ2 p= 0.43.
Conclusion: DCD pancreata are an underused resource that have the potential to increase the availability of islet cell transplant. We found no significant differences between islet cell isolation outcomes between DCD and DBD donors. While many donor factors show a strong correlation with absolute islet yield, it is impossible to use them ex-ante to determine if yield will meet the minimum yield of 200,000.
Lectures by Kenneth Nicoll
| When | Session | Talk Title | Room |
|---|---|---|---|
|
Sat-28 10:00 - 11:30 |
Islet transplantation: Extending islet donation and islet transplant "Potpouri" | 10-year experience of Donors after Circulatory Death for Islet Transplantation in Scotland | Indigo A |
