The pancreas after kidney transplant is the second-best option, comparable to the simultaneous pancreas and kidney transplant
ByungHyun Choi1, JeHo Ryu1, KwangHo Yang1, TaeBeom Lee1, JaeRyong Shim1.
1Surgery, Pusan National University Yangsan Hospital, Yangsan, Korea
Introduction: The simultaneous pancreas and kidney transplant (SPK) is the most common type of pancreas transplant performed worldwide. The number of pancreas after kidney transplants (PAK) in the United States has fallen since 2004 and has not yet returned to its previous level. There are a few drawbacks to PAK, such as the requirement for an additional operation, the immunologic risk for organs from different donors, the burden on the graft kidney resulting from two induction therapies and a higher tacrolimus dose, etc. SPK is the best option, but because to a lack of cadaveric donors and a lengthy waiting period, it is not always possible to use it.
Methods: From 2015 to 2022, we performed 21 PAKs at the Pusan National University Yangsan Hospital in Korea. 10 recipients received kidney transplants from living donors, while the remaining 11 received transplants from deceased donors. We compared the findings of PAK and SPK conducted within the same time period.
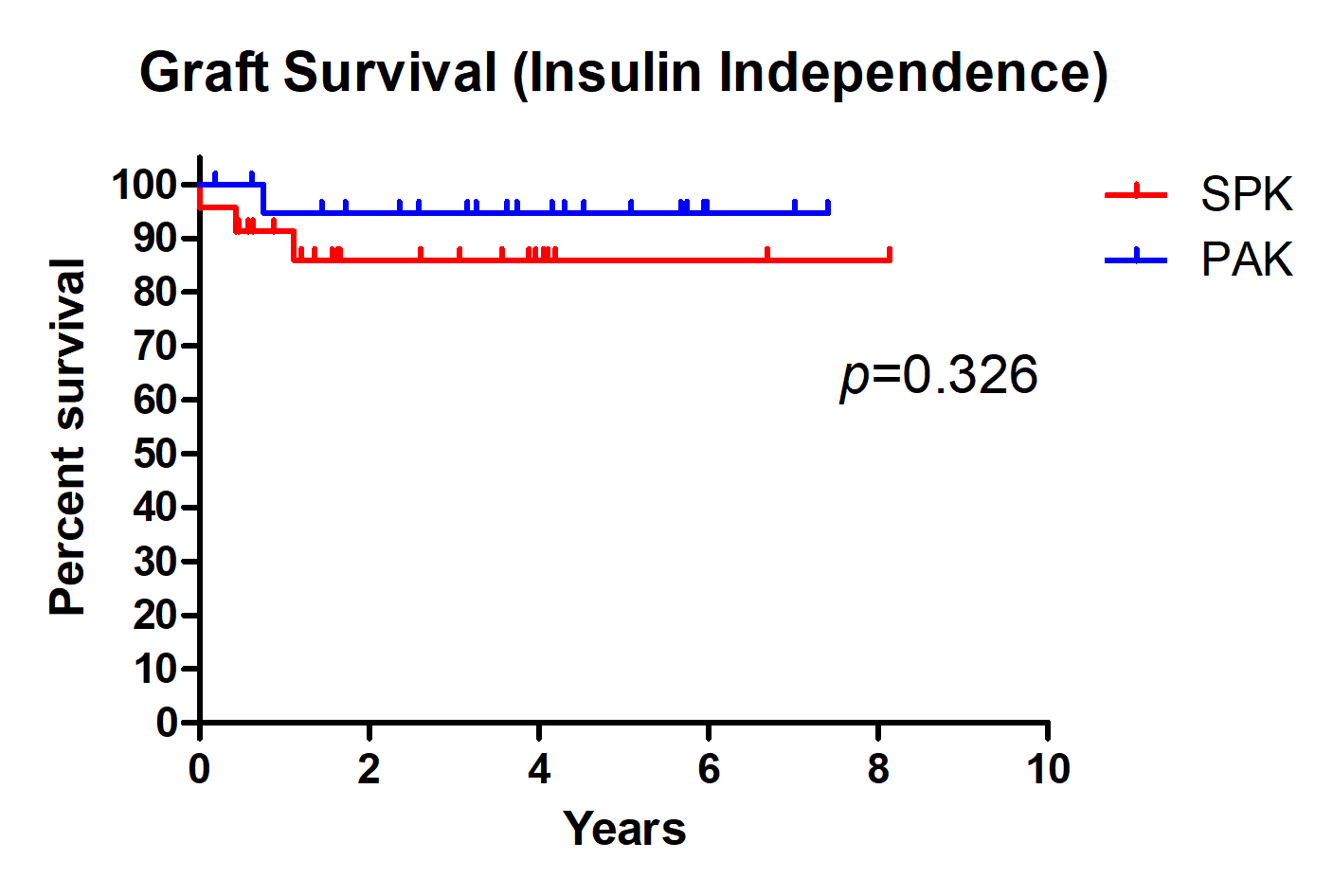
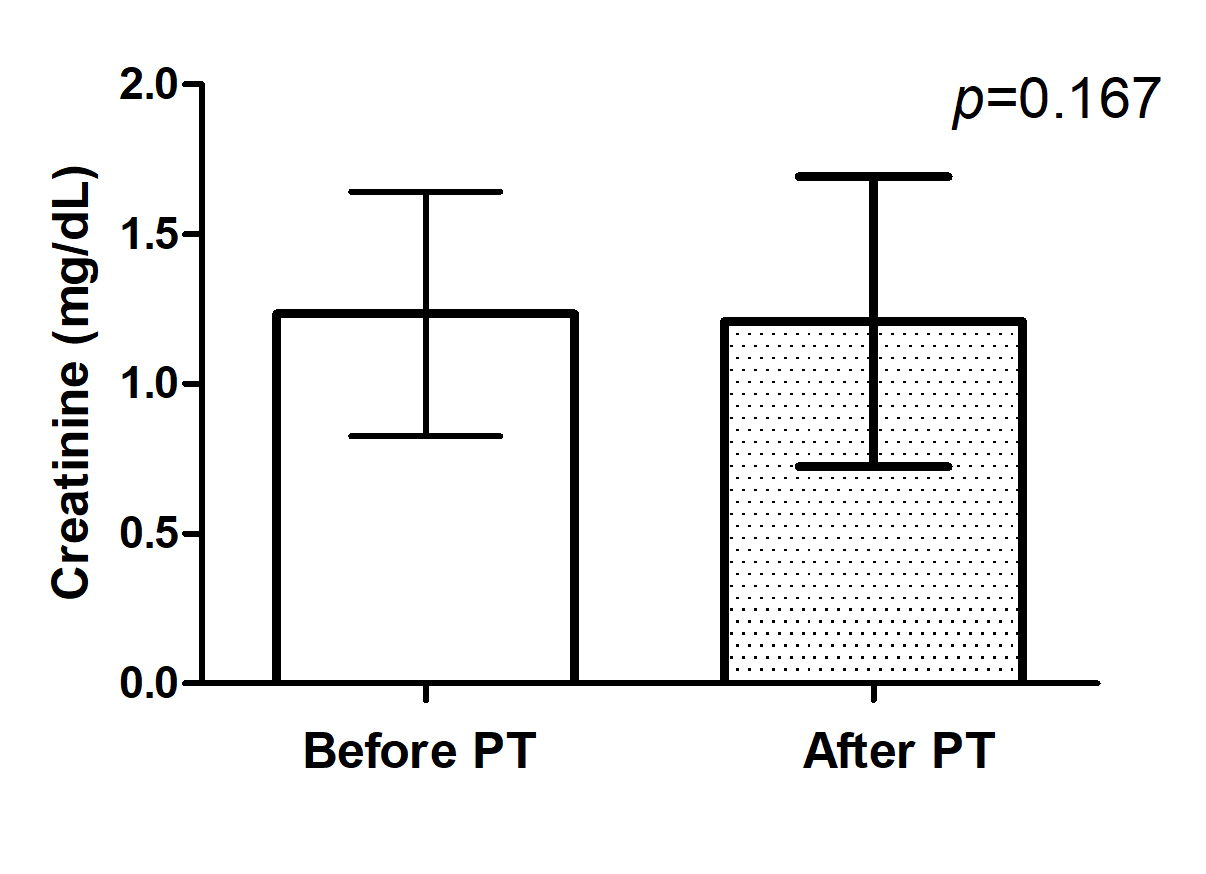
Results: Throughout the monitoring period, just one pancreatic graft was lost in PAK patients, and 7-year graft survival was 95%, with no statistically significant difference compared to SPK (87.5%, p=0.326). Moreover, the graft survival of SPK or PAK was superior to pancreatic transplant alone (PTA) (59.0%, p=0.022). Due to postoperative lymphoproliferative disease, the one pancreatic graft loss was a case of mortality with a functioning graft. No kidney transplant loss was observed in PAK recipients. Among PAK patients, there was no variation in creatinine levels between the pre-transplant and post-transplant periods. There were two incidents of pancreatic graft rejection, but the grafts entirely recovered following rejection treatment. Two kidney transplants were rejected, however the transplanted kidneys are salvaged after rejection treatment.
Conclusion: According to our experiences, PAK could be a second-best choice for individuals with diabetic end-stage renal disease, especially in cases where cadaveric donors were severely deficient but living donor kidney transplants were actively performed in countries like Korea.