Pancreas transplantation : Single center experience
Youngmin Ko1, Hyunwook Kwon1, Sung Shin1, Young Hoon Kim1, Duck Jong Han1.
1Department of Surgery, Asan medical center, Seoul, Korea
Background: The prevalence of diabetes in Korea is increasing steadily. Accordingly, the population suffering from diabetic complications is also increasing. Thus, the need for fundamental treatment of diabetes is emerging. Recently, with the development of novel immunosuppressants and the significant evolution in surgical methods of transplantation, pancreas transplantation has been introduced and successfully performed. Here we analyzed the outcomes of pancreas transplantation experienced over 28 years at a single center.
Methods: All recipients who underwent deceased donor or living donor PT from July 1992 to Dec 2020 were enrolled in this study. We reviewed their medical records, including operative records, as well as clinical and laboratory findings. We analyzed graft and patient survival rates using the Kaplan-Meier method.
Results: Four hundred eighty two cases were performed between July 1992 and Dec 2020. The indication for PT was type I diabetes in 334 (69.29%), and type II diabetes in 143 (29.6%) patients. The pancreas donor was deceased in 461 (95.6%) and living in 21 cases (4.3%).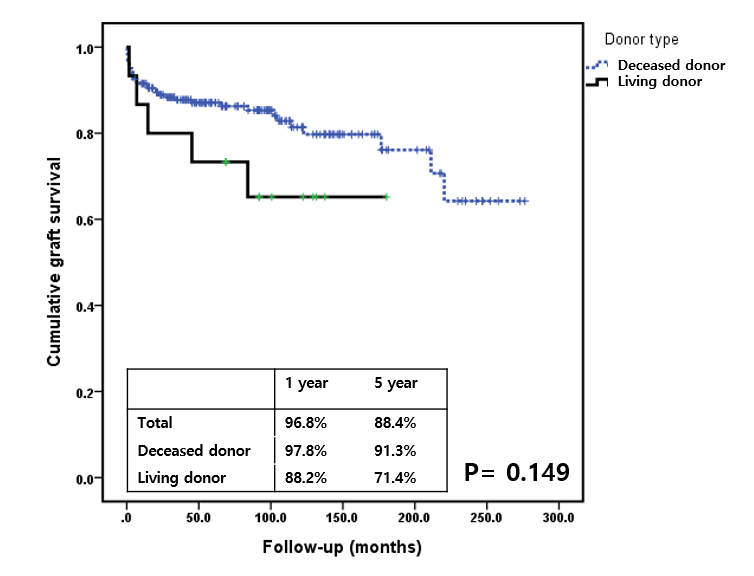
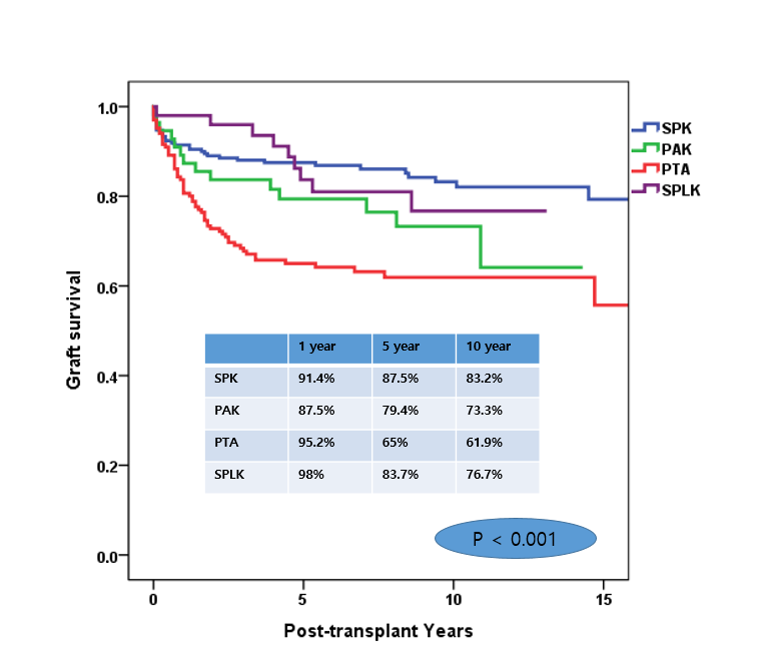
The type of PT was simultaneous pancreas-kidney transplantation (n = 210, 43.5%), pancreas alone (n = 167; 34.6%), or pancreas after kidney (n = 56, 11.6%), simultaneous deceased donor pancreas-living donor kidney transplantation (n = 49, 10.1%). Median follow-up was 90.0 months (range 0–367). At 1, 5, and 10 years overall patient survivals were 96.3%, 88.5%, and 71.9%, and graft survivals, 87.8%, 74.3%, and 56.0%, respectively. 1, 5 , 10 year pancreas graft survival rate showed a difference according to the type of surgery. Patient who underwent simultaneous pancreas-kidney transplantation had the superior survival rate, followed by simultaneous deceased donor pancreas-living donor kidney transplantation, pancreas transplantation after kidney transplantation, and pancreas transplant alone (P < .001).
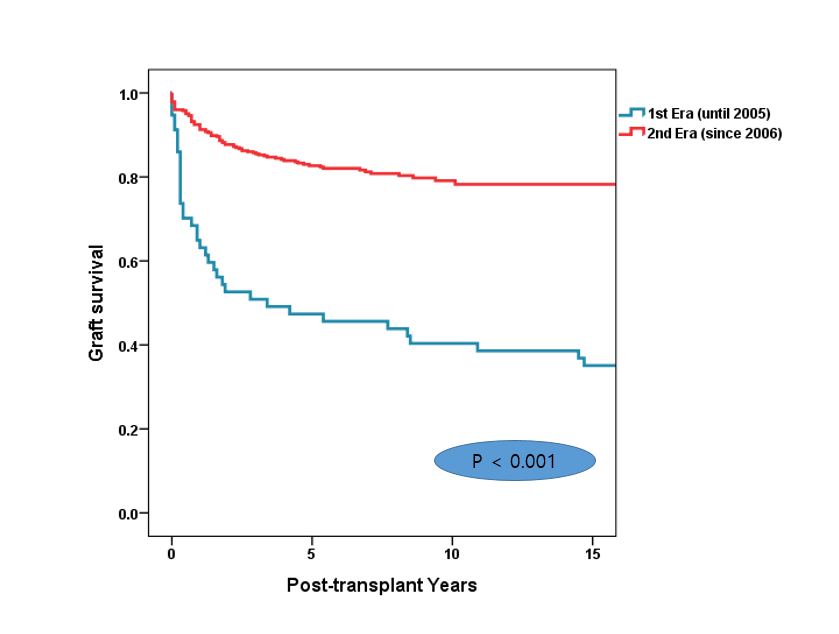
When we divided the deceased donor PT recipients into two groups according to when they underwent PT (up to 2006 [n = 57]) vs 2006 and later [n = 425]), the recent group showed significantly improved patient and graft survival rates (P < .001).
Conclusion: Considering the improved quality of life and long-term patient survival, pancreas transplantation can be an effective treatment option for diabetic patients.