Our first 50 pancreas transplants at a transplant program in Santiago de Chile
Javier Chapochnick1,2, Carlos Derosas1,2, Rodrigo Iñiguez1,2, Juan Gonzalez1, Jacqueline Pefaur3, Giovanni Enciso3, Marion Alarcon2, Andrea Canals4.
1Department of Surgery, Clinica Santa Maria, Santiago, Chile; 2Center for Organ Transplantation and Chronic diseases, Clinica Santa Maria, Santiago, Chile; 3Department of Nephrology, Clinica Santa Maria, Santiago, Chile; 4Academic Direction, Clinica Santa Maria, Santiago, Chile
Introduction: Until the opening of our pancreas transplant program in 2014 pancreas transplantation was anecdotal in Chile with an average number of cases per year of less than 1 and no existence of a national waiting list. The program in Clínica Santa María opened in 2014 aimed at treating patients from both the public and private health systems in our country.
Objective: The aim of this study is to share the growing experience of our pancreas transplantation program.
Methods: Retrospective cohort study that includes all pancreas transplants performed from March 2014 to November 2022 at Clinica Santa María. All patients have complete follow up (including of c-peptide, creatinine and glycosylated hemoglobin values). All recipient and donor demographics, type of transplant, immediate and late surgical complications, Covid-19 vaccination status, patient and graft survivals, and financial costs per transplant were analyzed. Logistic regression analysis of delayed graft function risk factors. Stata 14 was used for statistical analysis.
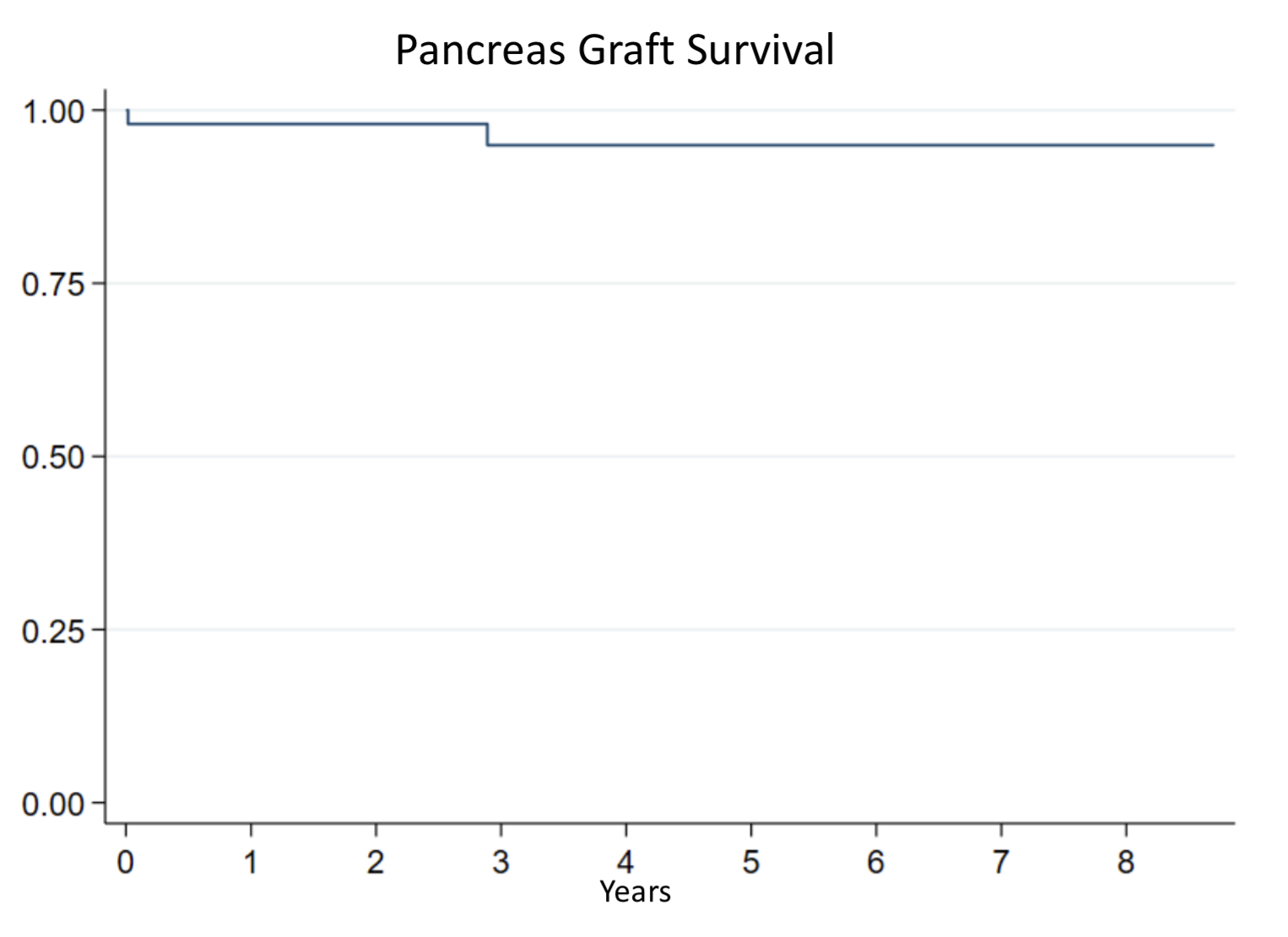
Results: Fifty transplants have been performed, 47 of them were simultaneous pancreas-kidney transplants (SPK) and 3 pancreas transplants alone (PTA). The indication for transplantation was DM1 in 46 patients (92%) and DM2 in 4 patients (8%). Most patients had chronic kidney disease and 80% were on renal replacement therapy at the time of transplant. All transplants were performed from deceased donors. Sixty percent of the patients were female, and the median age was 36.2± 7.6 years. The mean waiting time for transplantation was 24.6±14.7 months. Sixteen percent of the patients required a re-operation, hemoperitoneum being the most common cause (2 of 6). Delayed graft function (DGF) of the pancreatic graft was observed in 2 cases, one of them lost his pancreatic graft due to graft thrombosis. Five patients presented DFG of the kidney, two of them lost their kidney graft due to graft thrombosis. 88% of transplanted patients have completed Covid-19 vaccination status with at least 4 doses and only one patient died from Covid-19 pneumonia (vaccinated with 2 doses). Kaplan-Meier patient survival at one, three and five years is 100%, 92.4%, 92.4% respectively.
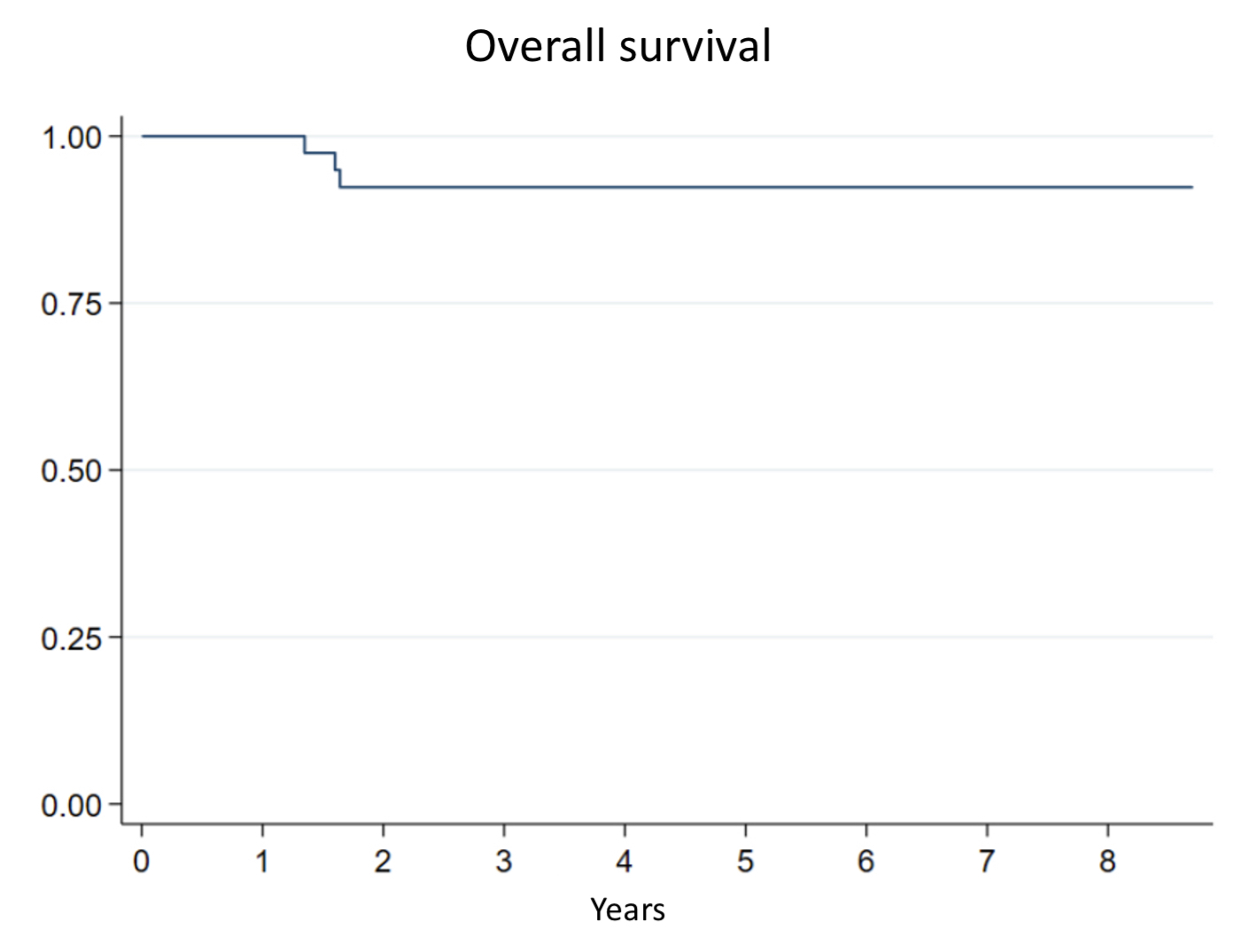
Death-censored graft survival for the kidney graft is 93.6%, 93.6%, 86% at 1, 3 and 5 years respectively. Death-censored graft survival for the pancreas graft is 98%, 94.9% and 94.8% at 1, 3 and 5 years respectively.
Discussion: This abstract shares the largest pancreas transplantation experience in Chile. Our young program has been growing and maturing and has become a real and tangible option for the diabetic patients of our country regardless of their health insurance.
[1] ALBA, ANDREA et al. Trasplante simultáneo de páncreas y riñon en diabetes mellitus tipo 1: Experiencia de un centro en Chile. Rev. méd. Chile . 2011, vol.139, n.1, pp.11-18
[2] Ferrario M et al. Trasplante simultaneo de pancreas y riñón. Conceptos actuales y experiencia en Clinica Las Condes. Revista Medica Clinica Las Condes Volume 27, Issue 2, 2016, Pages 179-187.
[3] Parajuli S, Arunachalam A, Swanson KJ, Aziz F, Garg N, Redfield RR, Kaufman D, Djamali A, Odorico J, Mandelbrot DA. Outcomes after simultaneous kidney-pancreas versus pancreas after kidney transplantation in the current era. Clin Transplant . 2019 Dec;33(12):e13732