
Video-assisted pancreas transplant debridement to manage peri-pancreatic abscess
Stuart Knechtle1, Brian Shaw1, Sabino Zani1, Paul Suhocki2.
1Department of Surgery, Duke University School of Medicine, Durham, NC, United States; 2Department of Radiology, Duke University School of Medicine, Durham, NC, United States
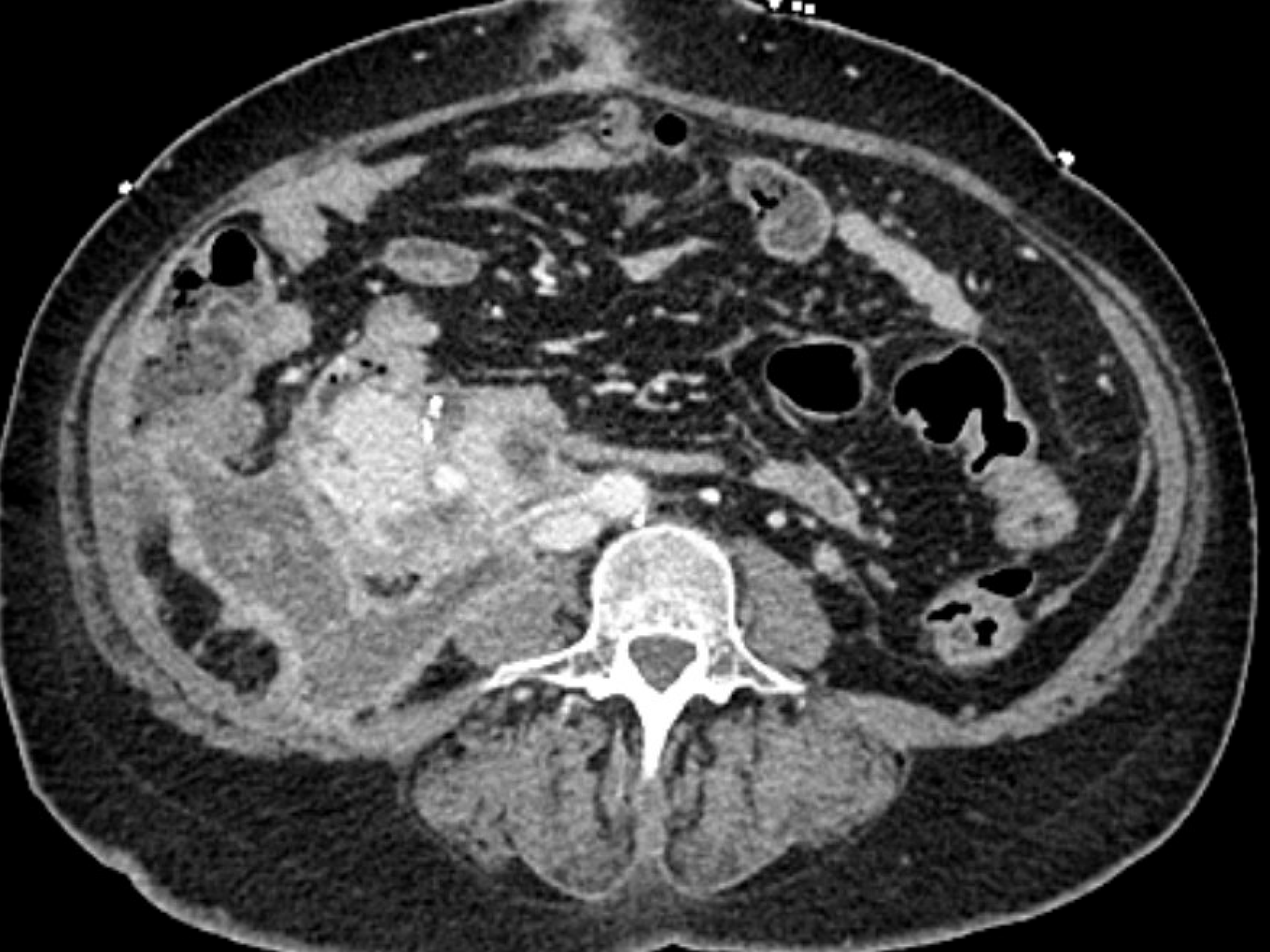
A 34 year old diabetic patient with end stage renal failure underwent combined pancreas-kidney transplantation and had early graft pancreatitis and delayed renal allograft function requiring laparotomy for bleeding after a kidney biopsy and two subsequent exploratory laparotomies for washout. She recovered good function of both pancreas and kidney but two months post-transplant developed a peri-pancreatic abscess as shown in the figure.
Despite percutaneous drainage and antibiotics to treat candida glabrata and enterobacter cloacae, she had undrained, persistent abscess by imaging with positive drain cultures. She underwent video-assisted retroperitoneal debridement and drainage of the abscess with debridement of a focus of infected, necrotic pancreas. With continued drainage and antibiotics, the abscess has resolved and she has maintained normoglycemia and normal renal transpant function (creatinine 0.6 ng/ml). We are not aware of previous use of video assisted retroperitoneal debridement/drainage of an abscess adjacent to a pancreas transplant, but our procedure is analogous to that used for native pancreatic necrosis with infection following pancreatitis. We found this procedure to be highly effective and avoided the potential morbidity associated with open laparotomy in this patient whose BMI was 32 and who had undergone 4 previous laparotomies. The patient was positioned in half lateral position to allow access along the track of the previously placed percutaneous drain. Insufflation of the abscess cavity initially with saline prior to trocar placment into the cavity provided a larger target for safe direction of the trochar, and insufflation of the cavity with CO2 provided good visualization using the camera, allowing debridement of the posterior aspect of the pancreas transplant, surrounding fat, and infected tissue. We recommend that this procedure be considered under similar clinical circumstances and that it requires advanced laparoscopic skills (such as coauthor S.Z.) to be done safely with judicious debridement. The patient has recovered well with good graft function of both pancreas and kidney transplants.