Analysis of islet isolation from DCD for allogeneic human islet transplantation to type1 diabetes – single center experience.
Gumpei Yoshimatsu1, Ryo Kawakami1, Teppei Yamada1, Naoaki Sakata1, Shohta Kodama1.
1Center for Regenerative medicine, Fukuoka University Hospital, Fukuoka, Japan
Introduction: In Japan, allogeneic human islet transplantation program was restarted under national medical insurance coverage in 2020. In our institution, 4 cases of islet transplantation was performed from 8 cases of islet isolation from donation after circulatory death (DCD), and 2 cases of islet transplantation was performed from 3 cases of islet isolation from the donation after brain death . The number of brain death donors is shortage in Japan, therefore islet isolation from DCD is still required to complete multiple times of islet transplantation. In this study, we aimed to demonstrate the analysis of the result of our institutional islet isolation from DCD.
Patients and Method: The 8 cases of islet isolation were divided into two groups; 4 cases of successful islet isolation (DCD-S) and 4 cases of failed islet isolation (DCD-F). The data were retrospectively analyzed as the experience of the single center.
Results: The DCD-S group had older age of donors than DCD-F (53.0±2.7yr, 35.0±8.8yr, respectively). Body weight was heavier in DCD-S than DCD-F (65.9±8.9kg, 51.7±0.9kg). Cold ischemic time was 431.5±54.5mins in DCD-S and 457.5±10.5mins in DCD-F. Pancreas weight was 84.0±5.8g in DCD-S and 64.6±7.6g in DCD-F. Post-digestive islet count was 550,421 ± 80,778 IEQ in DCD-S and 254,049 ± 27,670 IEQ in DCD-F. In DCD-S, 311,238±75,579 IEQ of isolated islets in 4.0 mL of pellet volume was transplanted into portal vein of patients as DCD-S. In the transplanted islets, the average of viability was 94.9±1.5% and purity was 45.0±5.0%. Post-digestive islet count was positively correlated with patient’s body weight (p=0.0006) and negatively correlated with cold ischemic time (p=0.069). Especially, the period between pancreas extraction and pancreas digestion was correlated with post-digestive islet yield.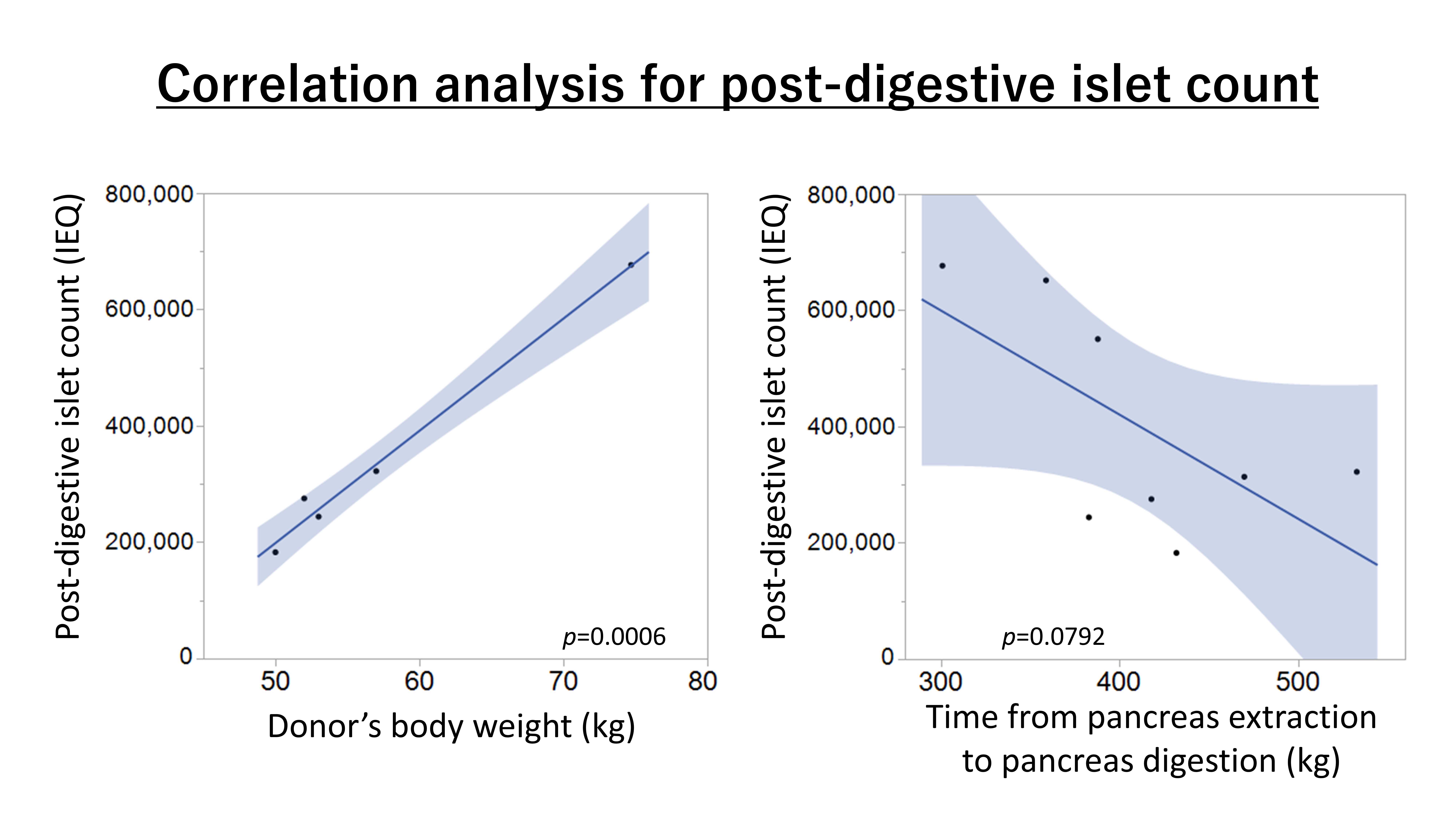
Discussion: Recently organ extraction from DCD has been attracted as controlled DCD, such as artificial circulation from ECMO. In the countries where DBD is shortage for the number of patients enrolling islet transplant program, DCD is still an essential donor source. The heavier body weight of donors and the shorter transporting time of extracted pancreas are the key of the successful islet isolation for the transplantation. In this study, the limitation is that the number of the islet isolation is still small for statistical analysis and that the metabolic outcome is not analyzed due to the small number and short follow-up period.
Conclusion: To determine the donor of pancreas, the body weight and the transporting time are important for the successful islet isolation for the islet transplantation.