
Solitary Pancreas Transplantation - Significant Improvement over the 2 last Decades
Angelika C. Gruessner1, Subodh J Saggi1, Rainer WG Gruessner1.
1SUNY Downstate Health Sciences University, Brooklyn, NY, United States
Introduction: Most pancreas transplants are performed in uremic and post-uremic diabetics. Pancreas Transplants Alone (PTAs) in non-uremic patients account for only 6-7% of pancreas transplants per year even though a PTA is the best treatment option to achieve long-term insulin-independence in patients with severe brittle diabetes and a relatively high risk of hypoglycemia-associated death.
Methods: We analyzed changes in demographics and outcome of 1,436 primary adult PTAs from deceased donors between 1/1/2002 and 12/31/2021 (two decades). Graft survival was defined as complete insulin-independence. Two recipient groups were studied: (1) < 35 and (2) ≥ 35 years of age. Multivariate analyses was performed to assess factors that impacted on short- and long-term outcome and the potential need for a subsequent kidney transplant.
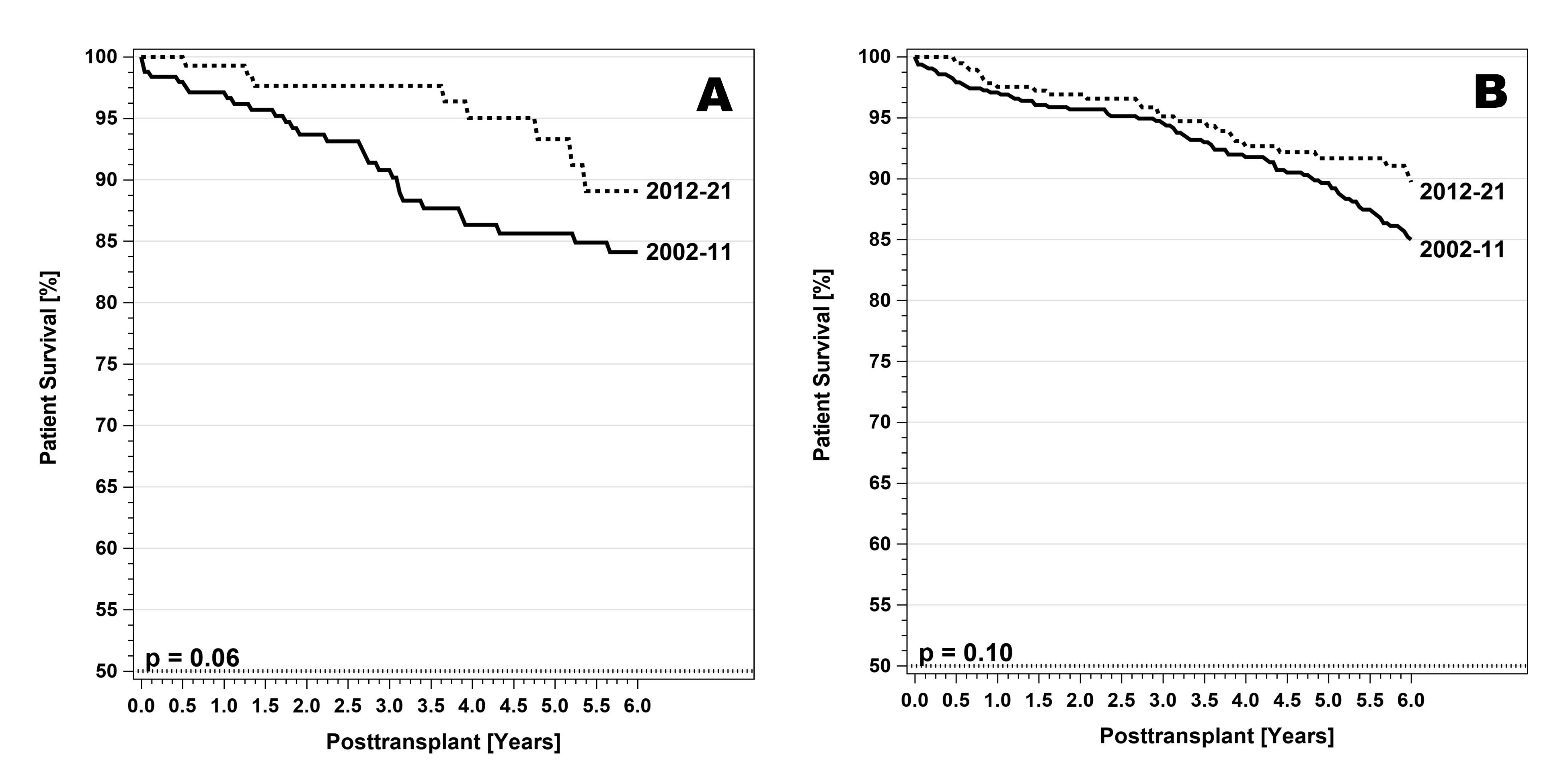
Results: The number of transplants decreased from 879 in the first to 551 in the second decade (-37%). Over time, recipient age, BMI, eGFR, increased, but donor age and preservation time decreased significantly. In the second decade most recipients received induction therapy with depleting antibodies and maintenance immunosuppression with tacrolimus and MMF. These changes resulted in significant improvements in patient and pancreas graft survival. Five-year patient survival for patients ≥ 35 years of age increased from 90% to 92% (p=0.10); for recipients <35 years, from 86% to 93% (p=0.06) (Figure 1)
Five-year pancreas graft survival for patients ≥ 35 years increased from 40% to 72%; for patients <35 years from 39% to 56% (p=0.01) (p=0.0001) (Figure 2).
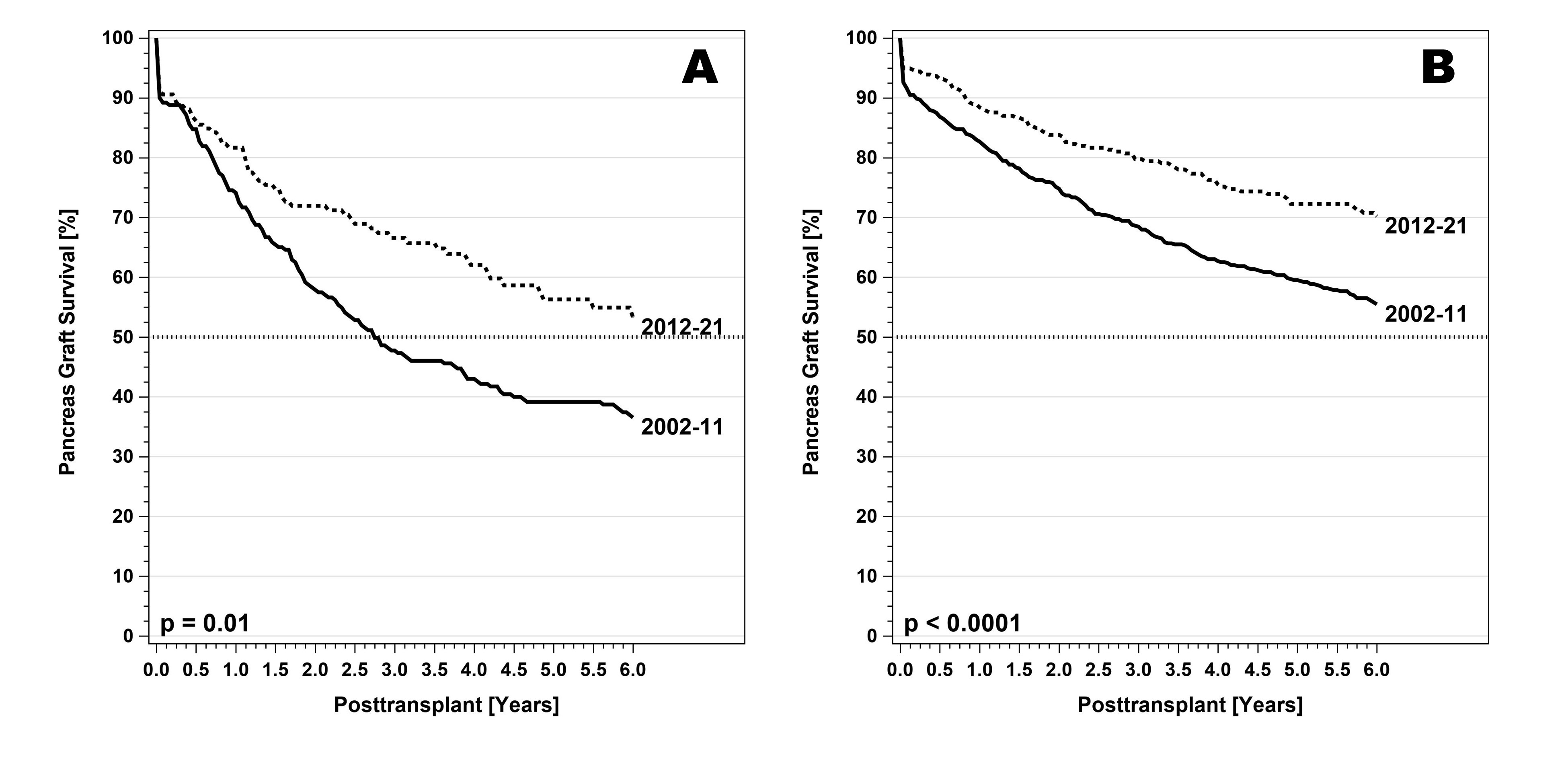
The early technical failure rate did not significantly change over time and remained stable around 6-7%. In contrast, the immunological graft loss rate in technically successful PTAs dropped significantly at 5-years both in recipients <35 and ≥ 35 years. A comparison between the two age groups showed that the 5-year immunological loss rate is significantly higher in younger recipients. By multivariate analysis, the most influential factors between the two groups were older recipient age and superior immunosuppression. Overall, the relative risk of pancreas graft loss decreased by 25%. Donor factors (age, preservation time, HLA matching) did not show any impact, possibly due to excellent donor selection. Transplants at high volume transplant centers showed significantly better outcome.
Due to better donor and recipient selection, refinements in immunosuppression, and improvements in graft outcome, the rate of a subsequent kidney transplant declined significantly. This rate was primarily contingent on native graft function at the time of the pancreas transplant. If the GFR was >80/min, only 3% of patients had received a kidney graft 5-years after PTA.
Discussion/Conclusion: This study shows that (1) the results of PTA have significantly improved over the past 20 years; (2) a PTA should be strongly considered in brittle diabetic patients before the development of advanced diabetic complications; (3) although the risk of immunological failure has also significantly decreased, results are still best in recipients ≥ 35 years of age.