Demand prevalence on health care services by type 1 and 2 diabetes mellitus in an Australian population – a data linkage analysis
Rohan Bhattacharjya1, Tristan J Bampton1, Meg Barnett2, Lyle J Palmer1, Toby P Coates1,2.
1Medical School, University of Adelaide, Adelaide, Australia; 2CNARTS, Royal Adelaide Hospital, Adelaide, Australia
Aim: To obtain contemporaneous prevalence data on demand for healthcare services in South Australia for types 1 and 2 diabetes.
Introduction: Diabetes is a significant healthcare problem in Australia. Studies quantifying the demand on health care systems using local data have not been conducted. Difficulties with conducting any such study include their retrospective nature, incomplete datasets, that do not factor the impact of changing practice in medicine and do not account for changing therapeutics.
Methods: A comprehensive data set was obtained from SA-NT Datalink, based on hospital discharge ICD-10 codes and covering all-cause hospital interactions from 1999 to 2023. Data from 01-01-2017 to 31-12-2022 was analysed. Patients were classified into 3 groups: General Population, Type 1 Diabetes Mellitus (T1DM), and Type 2 Diabetes Mellitus (T2DM). Data on patient demographics, requirements for in-hospital admission and requirement for ICU admission were analysed. Chi-squared test was used where appropriate and a p<0.05 was considered significant.
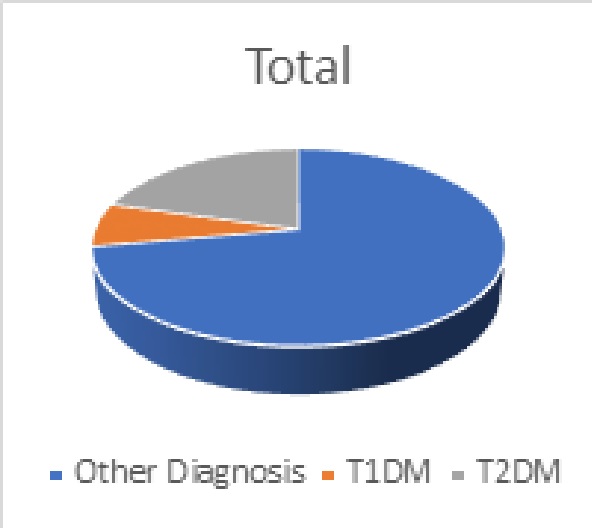
Results: 7800 individual patients and all their hospital interactions between 01-01-2017 and 31-12-2022 were analysed. 559 (7.2%) of these patients had T1DM and 1609 (20.6%) had T2DM. The remainder were non-diabetic (Figure 1).
The age and sex distribution of the chosen cohort mirrored that of the general population in South Australia.
While there was a significant number where the data was not available there was a proportionate representation of patients of indigenous origin in this cohort (3.4% in the chosen cohort against 2.4% in the South Australian Census).
As a proportion, the need for in-hospital care was significantly more significant as compared to out-patient or ambulatory care in patients who were diabetic as compared to non-diabetic (p0.0005)(Figure 2a)
There was no difference in the need for ICU admission between the 3 cohorts studied (Figure 2b).
Conclusions: These data suggest that though Diabetics represent only 30% of the total population of hospital admissions their need for in-hospital care is greater than non-diabetic patients. Using data linkage provides a unique means to understand the impact that Diabetes has on patient care needs. Dissecting contemporary trends in health utilization have important implications for T1D and T2D and future planning for Health Care services into the future.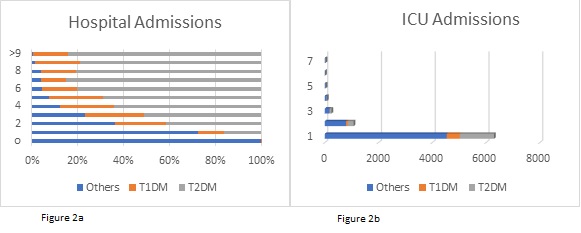
[1] Comino, E.J., Harris, M.F., Islam, M.F. et al. Impact of diabetes on hospital admission and length of stay among a general population aged 45 year or more: a record linkage study. BMC Health Serv Res 15, 12 (2015). https://doi.org/10.1186/s12913-014-0666-2
[2] Choi J, Booth G, Jung HY, Lapointe-Shaw L, Tang T, Kwan JL, Rawal S, Weinerman A, Verma A, Razak F. Association of diabetes with frequency and cost of hospital admissions: a retrospective cohort study. CMAJ Open. 2021 Apr 16;9(2):E406-E412. doi: 10.9778/cmajo.20190213. PMID: 33863799; PMCID: PMC8084549.