Cost Savings Using The BETA-2 Versus Beta Score In Follow-Up Of Islet Transplant Recipients In The UK Islet Transplant Consortium.
Aileen Nielson1, John Casey2, Andrew Sutherland2, Miranda Rosenthal3, Sufyan Hussain4, Maria De Los Angeles5, Martin Rutter6,7, David vanDellen8, Hussein Khambalia8, Shazli Azmi8, Alistair Lumb9, Paul Johnson10, James Shaw5,11, Shareen Forbes2,12.
1Edinburgh Clinical Trials Unit, Usher Institute, University of Edinburgh, Edinburgh, United Kingdom; 2Transplant Unit, Royal Infirmary of Edinburgh, Edinburgh, United Kingdom; 3Department of Diabetes Services, Royal Free London NHS Foundation Trust, London, United Kingdom; 4Department of Diabetes, School of Cardiovascular, Metabolic Medicine and Sciences, King's College London, London, United Kingdom; 5Diabetes and Endocrinology , The Newcastle upon Tyne Hospitals NHS Foundation Trust, Newcastle upon Tyne, United Kingdom; 6Diabetes, Endocrinology and Gastroenterology, School of Medicine, Faculty of Biology, Medicine and Health, University of Manchester, Manchester, United Kingdom; 7Diabetes, Endocrinology and Metabolism Centre, Manchester NIHR Biomedical Research Centre, Manchester University NHS Foundation Trust, Manchester, United Kingdom; 8Department of Renal & Pancreas Transplantation, Manchester University NHS Foundation Trust, Manchester, United Kingdom; 9Department of Diabetes , Oxford University Hospitals NHS Foundation Trust, Oxford, United Kingdom; 10Nuffield Department of Surgical Science, University of Oxford, Oxford, United Kingdom; 11Translational and Clinical Research Institute, Newcastle University, Newcastle, United Kingdom; 12Centre for Cardiovascular Science, Queen's Medical Research Institute, University of Edinburgh, Edinburgh, United Kingdom
Introduction: Traditionally the beta score, derived from a standard 90-minute mixed meal tolerance test (MMTT) stimulated C-peptide concentration, fasting glucose, HbA1c and insulin dose, is used to monitor graft function in the UK Islet Transplant Consortium (UKITC). The BETA-2 score is a validated refinement of the beta score but is calculated from a fasting C-peptide with no requirement for a MMTT. We aimed to perform an economic analysis to explore potential cost savings using the BETA-2 score instead of the beta score in islet transplant recipients in the UKITC.
Methods: The cost analysis examined n=28 patients with Type 1 diabetes receiving an islet transplant in 2018/19 (Islet Transplant Alone=20 and Simultaneous Islet Kidney Transplants=8) calculated from time of transplantation to 12 months after. The unit costs of hospital outpatient visits were derived from published NHS Reference Costs. Cost of an outpatient follow-up visit involving MMTT (£497) was based on the non-consultant led non-admitted face-to face attendance; an out-patient visit that did not require a MMTT (£253) was based on the reported reference cost for consultant-led Multiprofessional Non-Admitted Face-to-Face Attendance.
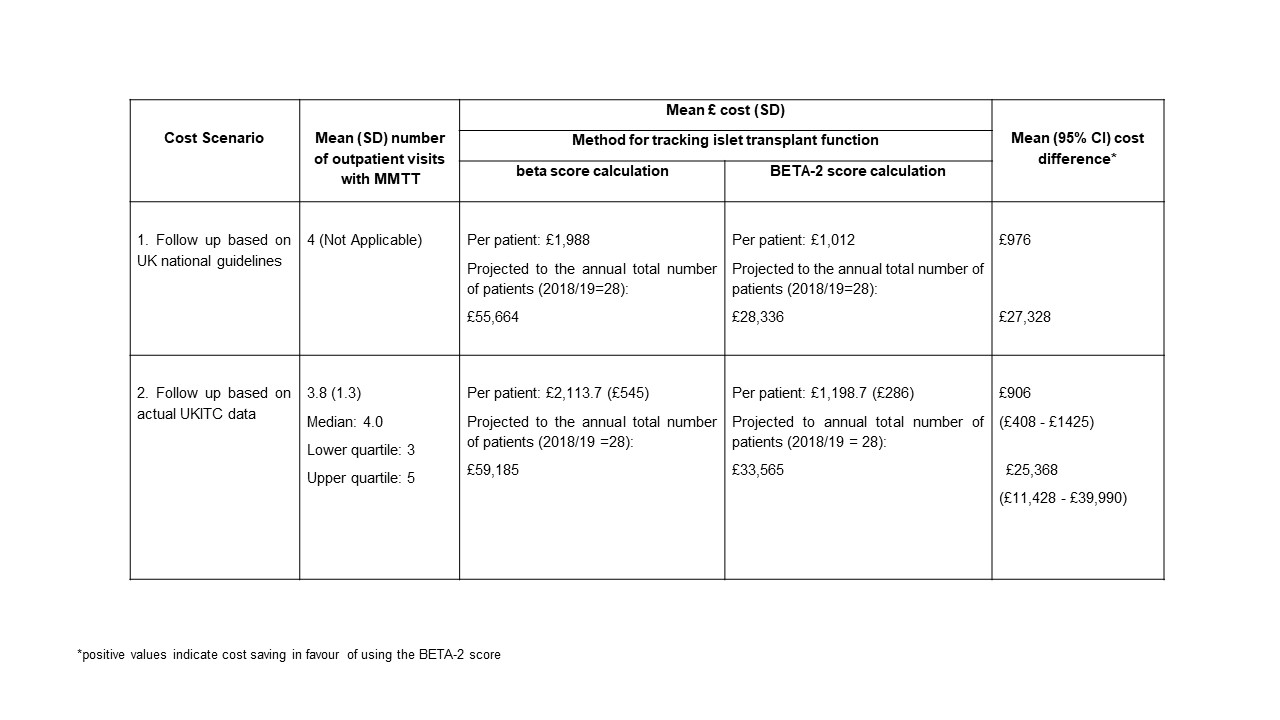
Two costing scenarios were explored:
1) Mean follow-up cost per patient as per the recommendations of National guidelines on assessment after 1st islet transplantation (assumption of 4 visits in first year) with total costs based on 28 patients in the year 2018/19.
2) Mean follow-up cost per patient was calculated using the actual follow-up data (i.e. observed number of visits in first year post transplant) from the UKITC transplant registry patients (2008-2015): based on 84 transplant recipients including 14 recipients who lost graft function within 12 months.
In both scenarios, calculations included the mean differences in follow-up costs using the BETA-2 scores versus beta-scores (using non-parametric bootstrapping with 1000 replicates for scenario 2). Costs were applied to patient numbers receiving transplants in 2018/19 (i.e. 28 patients).
Costs were expressed in UK pounds sterling (£) at 2018/19 prices. No discounting of hospital costs was undertaken.
Results: After 12 months using the BETA-2 vs. beta score, the mean (95% CI) cost saving per patient was predicted to be £906; (95% CI [£408 - £1,425]) (Table 1, based on the observed/actual number of follow-up visits, i.e. scenario 2). For the 28 patients receiving transplants annually in 2018/19, the mean (95% CI) cost saving in the first year following transplantation was predicted to be £25,368 (95% CI: [£11,428 - £39,990]).
Conclusions: We demonstrate potential cost savings using the BETA-2 versus the beta score for monitoring islet graft function. We believe that these cost saving estimates are likely to be conservative and applicable to other islet transplant programmes.
This research is supported by the UKITC extended clinical and allied research teams. The analyses were supported from a grant award from the University of Edinburgh..
[1] E. A. Ryan, B. W. Paty, P. A. Senior, J. R. Lakey, D. Bigam and A. M. Shapiro, "Beta Score: an assessment of beta cell function after islet transplantation". Diabetes Care 2005 Vol. 28 Issue 2 Pages 343-7
[2] S. Forbes, R. A. Oram, A. Smith, A. Lam, T. Olateju, S. Imes, A. J. Malcolm, A. M. J. Shapiro, P. A. Senior, "Validation of the BETA-2 Score: An Improved Tool to Estimate Beta Cell Function After Clinical Islet Transplantation Using a Single Fasting Blood Sample". Am J Transplant 2016 Vol. 16 Issue 9 Pages 2704-13