Cardiovascular events in subjects after islet transplantation
Joana Lemos1, Raffaella Pogiolli1, David Baidal1, Ana Alvarez1, Camillo Ricordi1, Rodolfo Alejandro1.
1Clinical Cell Transplant Program - Diabetes Research Institute (DRI), University of Miami, Miami, FL, United States
Introduction: Intensive glycemic control improves long-term cardiovascular outcomes in subjects with diabetes. Islet transplantation (ITx) is a safe procedure for Type 1 Diabetes (T1D), and it provides benefits on microvascular complications, but the chronic use of immunosuppression (IS) has been associated with several adverse effects, some of them associated with increased cardiovascular risk, including changes in blood pressure and lipid metabolism. We aimed to determine the incidence rate of cardiovascular events (CVEs) in subjects after ITx and evaluate its association with clinical and metabolic factors.
Methods: A cohort of 56 patients with T1D was followed-up for 20 years. Patients received islets via intrahepatic portal infusion (n=53) or via omental approach (n=3). The outcomes included major cardiovascular events, such as acute myocardial infarction, stroke, or heart failure. CVE rates were calculated per 1,000 person-years. Analyses of association according to CVE presence among variables were performed using Fisher’s exact test. Metabolic evaluation along time and between subjects was investigated through generalized linear model for repeated measures. P <0.05 were considered statistically significant.
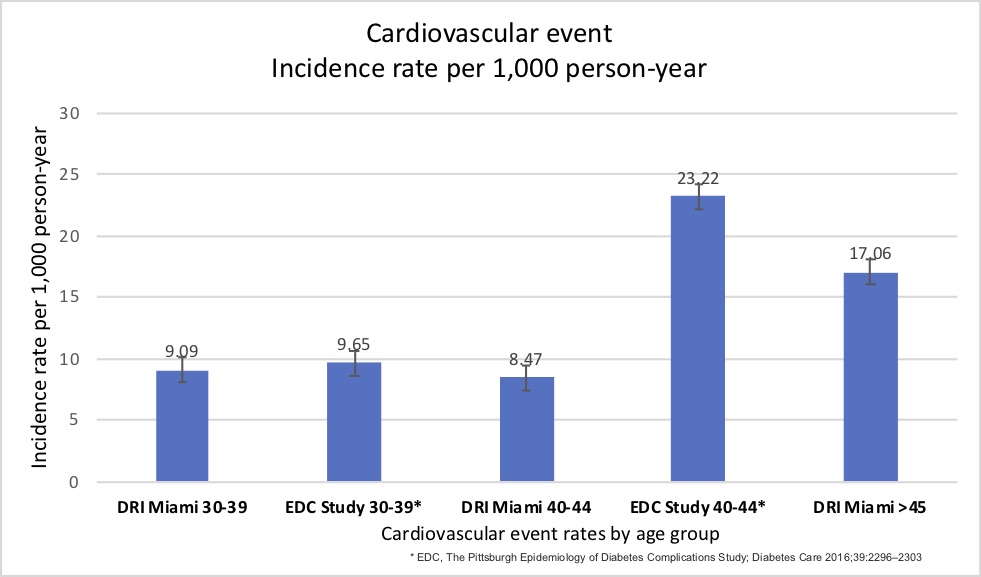
Results: Out of 56 patients, 8 (14.3%) presented CVE, and 3 (37.5%) had residual graft function at the time of event. Median time from first ITx until the occurrence of CVE was 133 (67 – 225) months. Age at CVE was 47±8.7 years, and 37.5% (n = 3) were female. In subjects who had CVE, mean BMI at ITx was 23.85±1.45kg/m2 and by the end of follow-up was 23.62±3.05kg/m2, which is not different from the BMI in subjects without CVE (P=0.509). Young adults aged 30–39 years had a CVE rate of 9.09/1,000 person-years (95% CI 2.3 - 50), those aged 40–44 years had a rate of 8.47/1,000 person-years (95% CI 2.15 - 47), and subjects aged >45 had a rate of 17.05/1,000 (95% CI 9.19 – 41) person-years. The Pittsburgh Epidemiology of Diabetes Complications Study Cohort reported a higher incidence rate of CVE in T1D in comparison of our cohort, considering the same age groups.
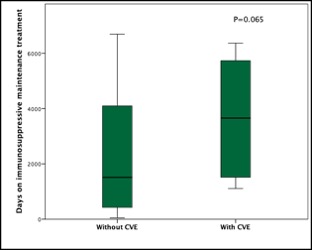
Time on IS treatment was similar between patients with or without CVE.
CVE was not associated with graft status, sex, BMI, type of transplant (Islet Alone or islet after kidney), or presence of albuminuria. Lipid profile and HbA1C were similar between the groups.
Conclusion: In subjects who undergone ITx the incidence of cardiovascular events seems to be reduced in comparison to previously reported patients with T1D in the same age groups. CVE did not differ in patients regardless of the graft function status, previous kidney transplant, or time on IS, suggesting that immunosuppression may not play a role on the incidence of CVE in this population. Further prospective studies with surrogate markers for cardiovascular disease should be considered for better understanding the cardiovascular outcomes after ITx.
This study was supported by NIH grants R01 DK55347, R01 DK056953, R01 DK025802, DK070460, U42 RR016603, M01RR16587, UL1TR000460; the Miami Clinical and Translational Science Institute (CTSI) from the National Center for Advancing Translational Sciences and the National Institute on Minority Health and Health Disparities; the Juvenile Diabetes Research Foundation International 4-200-946, 4-2004-361, 17-2012-361, 3-SRA-2017-347-M-B; the State of Florida; and the Diabetes Research Institute Foundation. The authors are grateful to the members of the cGMP Human Cell Processing Facility, the pre-clinical Human Immunology and Immunogenetics Program, the Clinical Cell Transplant Program (CCTP) at the Diabetes Research Institute (DRI), and the University of Miami CTSI for their support of this work. .
[1] Miller RG, Mahajan HD, Costacou T, Sekikawa A, Anderson SJ, Orchard TJ. A Contemporary Estimate of Total Mortality and Cardiovascular Disease Risk in Young Adults With Type 1 Diabetes: The Pittsburgh Epidemiology of Diabetes Complications Study. Diabetes Care. 2016 Dec;39(12):2296-2303. doi: 10.2337/dc16-1162. Epub 2016 Sep 21. PMID: 27654986; PMCID: PMC5127232.
[2] Shapiro AM, Pokrywczynska M, Ricordi C. Clinical pancreatic islet transplantation. Nat Rev Endocrinol. 2017 May;13(5):268-277. doi: 10.1038/nrendo.2016.178. Epub 2016 Nov 11. PMID: 27834384.
[3] Fiorina P, Gremizzi C, Maffi P, Caldara R, Tavano D, Monti L, Socci C, Folli F, Fazio F, Astorri E, Del Maschio A, Secchi A. Islet transplantation is associated with an improvement of cardiovascular function in type 1 diabetic kidney transplant patients. Diabetes Care. 2005 Jun;28(6):1358-65. doi: 10.2337/diacare.28.6.1358. PMID: 15920052.