Is Therapeutic Protein Leakage from Membranous Nephropathy a Factor in the Rejection of Pig Kidneys?
Kohei Kinoshita1, Ivy A Rosales1,2, Akihiro Maenaka1, Ira Doressa Anne How2, Martin Karl Selig2, Christina Laguerre2, Bernard A Collins2, David Ayares3, Robert B Colvin1,2, David K Cooper1.
1Center for Transplantation Sciences, Department of Surgery, Massachusetts General Hospital/Harvard Medical School, Boston, MA, United States; 2Department of Pathology, Immunopathology Research Laboratory, Massachusetts General Hospital/Harvard Medical School, Boston, MA, United States; 3Revivicor, Inc, Blacksburg, VA, United States
Introduction: Blockade of co-stimulation pathways by monoclonal antibody therapy has prolonged gene-edited pig graft survival in nonhuman primates (NHPs). However, the optimal regimen (dose, dosing schedule, therapeutic trough level) remains uncertain. Membranous nephropathy causes nephrotic syndrome with loss of high molecular weight proteins, specifically IgG. Our hypothesis is that this may lead to reduced trough levels of therapeutic anti-CD154mAbs.
Methods: A kidney from a double-knockout (GGTA1/B4GalNT1) pig with additional GHR-KO and expression of six human protective proteins was transplanted into a baboon. Induction immunosuppressive therapy consisted of anti-thymocyte globulin, rituximab, and a C1-esterase inhibitor. Maintenance therapy consisted of an Fc-modified anti-CD154mAb and rapamycin, but no corticosteroids. Complete blood counts, serum creatinine, blood urea nitrogen, serum total protein and albumin, and urine creatinine and protein levels were monitored.
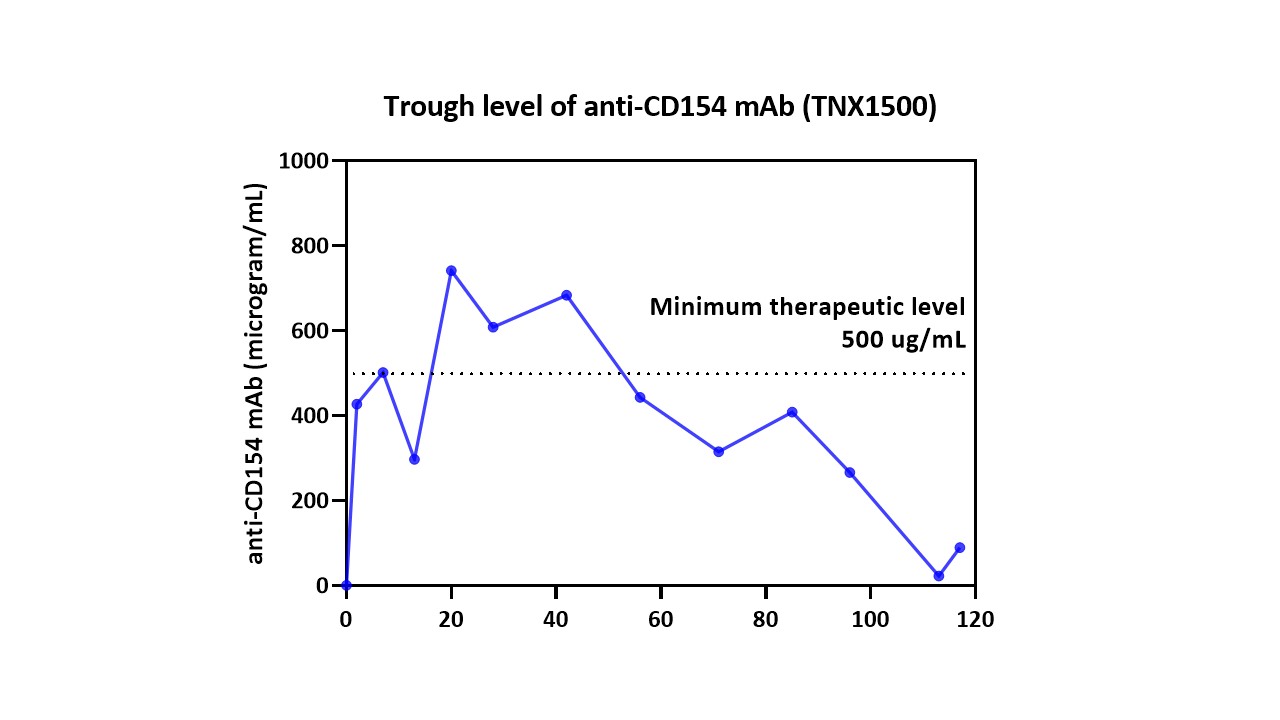
Results: Until day 42, the serum creatinine remained stable (1.0mg/dL) but proteinuria developed. A kidney biopsy on day 43 showed acute thrombotic microangiopathy (TMA) involving 30% of the glomeruli, with diffuse C4d deposition along the peritubular capillaries. A biopsy on day 71 showed acute TMA in only 20% of the glomeruli (with C4d deposition). Because rapamycin therapy can be associated with TMA, we discontinued rapamycin therapy. Urine protein levels remained elevated, and the serum total protein and albumin levels decreased to 1.5g/dL. After this, the serum creatinine increased to 3.4mg/dL, and the platelet count fell to 30,000/µL. An emergent biopsy on day 111 showed TMA in 80% of the glomeruli, diffuse peritubular capillaritis, and peritubular capillary C4d deposition, consistent with acute antibody-mediated rejection (AMR). Despite bolus steroid therapy and the resumption of rapamycin, the serum creatinine progressively rose, and the animal was euthanized on day 120. Electron microscopy of kidney tissue performed retrospectively at three time-points (pre-transplant, day 111, and day 120) revealed membranous nephropathy on day 111. Retrospective measurements of the trough levels of the anti-CD154 mAb showed a continuing fall to subtherapeutic levels from day 56 (Figure 1).
Conclusions: We hypothesize that the development of membranous nephropathy (which may have been a feature of low-grade AMR) was associated with increasing proteinuria and a concomitant fall in the trough levels of the therapeutic protein, anti-CD154mAb. This, in turn, together with the (incorrect) discontinuation of rapamycin therapy, enabled AMR to develop rapidly, resulting in graft failure. We conclude that the serum levels of anti-CD154mAbs should be measured throughout the post-transplant course, particularly if proteinuria has developed, and the dosage adjusted to maintain an effective trough level.